Home » Cancer Types » Lung & Thoracic Cancer
Lung & Thoracic Cancer
- Overview
- Treatment Options
- What to Expect
Lung cancer is the leading cause of cancer deaths in both men and women in the United States. According to the American Cancer Society, this year nearly 175,000 Americans will learn they have lung cancer.
The primary risk factor for lung cancer is smoking which accounts for more than 85% of all lung cancer related deaths. The risk of lung cancer increases with the number of cigarettes smoked per day as well as the number of years spent smoking. Exposed non-smokers have an increased relative risk of developing lung cancer as well. There is a 20 to 30 percent increased risk for lung cancer associated with living with a smoker. Other risk factors include exposure to substances like radon gas, asbestos, polycyclic aromatic hydrocarbons, chromium nickel organic arsenic compounds, recurrent lung inflammation, and lung scarring secondary to tuberculosis.
Symptoms of Lung Cancer
Most lung cancers do not cause symptoms until they have gotten quite large or have spread. Some of the most frequent symptoms due to growth of the cancer in the lung are:
- A persistent cough, chest pain, bloody sputum.
- New onset of wheezing, shortness of breath, recurrent infections such as bronchitis and pneumonia.
- Shoulder pain with numbness in some fingers with or without a droopy eyelid.
- Hoarseness.
- Unexplained weight loss, loss of appetite.
- Fatigue.
In many cases, lung cancer may have spread to distant organs before it causes any symptoms. Symptoms caused by cancer that has spread to other organs include:
- Bone pain
- Weakness or numbness of the arms or legs
- Dizziness
- Seizures
Workup
The medical history and physical exam are the first steps toward finding out whether a lung cancer is present and how far it has spread. A chest x-ray will often reveal a tumor. Other imaging tests such as CT scans and PET/CT scans may provide more detailed information about the extent of your tumor and it’s location in the lung. Depending on the results of the imaging tests, one or more of the following procedures may be used to collect samples that are checked for cancer cells.
- Sputum cytology: a sample of phlegm is checked to see if cancer cells are present
- Fine needle biopsy: a thin needle is used to biopsy the suspicious area in the lungs to obtain a piece of tissue. The biopsy is done with the needle inserted through the skin into the suspicious area in the lungs under fluoroscopy or CT guidance
- Bronchoscopy: a lighted flexible tube called a bronchoscope, is passed through the nose into the bronchus to help find tumors and take samples of tissue or fluids and to thoroughly check the lining of the other airways in the lungs
- Mediastinoscopy: with the patient under general anesthesia, a lighted tube is inserted under the breastbone through a small cut in the base of the neck to obtain a tissue sample from the nodes in the middle of the chest
- Thoracentesis: This procedure is done to check whether fluid around the lungs is caused by cancer cells that have spread to the pleural membranes or the lining of the lungs
Types of Lung Cancer
Non-Small Cell Lung Cancer
This is the most common type of lung cancer accounting for 85 to 90 percent of lung cancers. There are three subtypes within this group
- Squamous cell carcinoma
- Adenocarcinoma (including bronchoalveolar carcinoma)
- Large cell undifferentiated carcinoma
Small Cell Lung Cancer (SCLC)
This type accounts for 10 to 15 percent of all lung cancers. Other names for small cell lung cancer are oat cell cancer, small cell undifferentiated carcinoma, and poorly differentiated neuroendocrine carcinoma.
Other Types of Lung Cancer
This includes malignant mesothelioma; a type of cancer that develops from the cells of the pleura or lining of the lung.
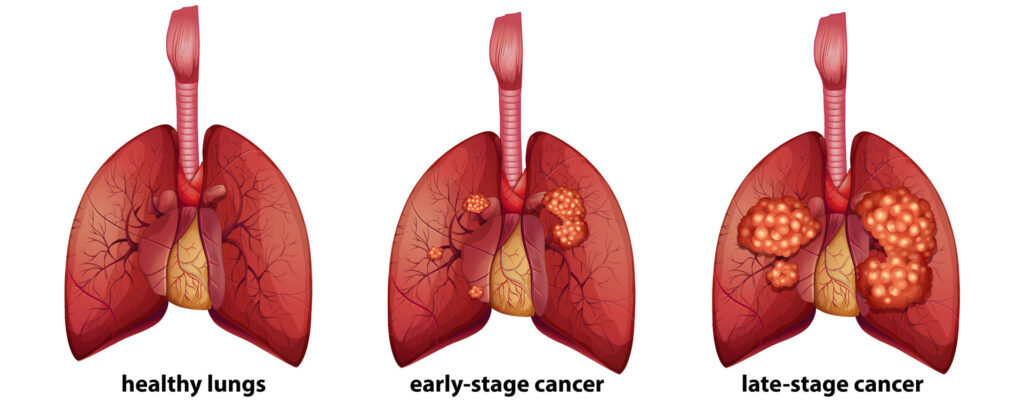
Lung Cancer Staging
Staging is the process of finding how far the cancer has spread. This is very important because your treatment and your prognosis depend, to a large extent, on your cancer’s stage as well as cell type. Tests, such as CT, MRI, PET/CT, mediastinoscopy, bone marrow biopsy, and blood tests are used to stage the cancer.
Staging of Non-Small Cell Lung Cancer
The system most often used to describe the growth and spread of non-small cell lung cancer is the TNM staging system. This is also known as the American Joint Committee on Cancer (AJCC) system. In this staging system, information about the tumor, nearby lymph nodes, and distant organ metastases is combined and a stage is assigned to a specific TNM grouping. T stands for tumor, its size, and how far it has spread within the lung into nearby organs. N stands for spread to lymph nodes. M stands for metastases or spread to distant organs. The group stages are described using the number 0 and Roman numerals from I to IV.
Staging of Small Cell Lung Cancer
A much simpler two stage system works better in selecting treatment options for small cell lung cancer. The system divides small cell lung cancer into “limited stage” and “extensive stage.”
- Limited stage means the cancer is only in one lung and in lymph nodes in the same side of the chest.
- Extensive stage means the cancer has spread to the other lung or to lymph nodes in the other side of the chest, or to distant organs or if there is malignant fluid surrounding the lung.
Types of Treatment for Lung Cancer
Lung cancer treatment planning is very complex. A team of cancer care doctors may be involved in the decision making process, including a radiation oncologist, medical oncologist, and a surgeon. The appropriate cancer treatment depends on several factors including the type and size of the cancer, its location, your overall health, and performance status. Often, several different treatments and combination of treatments will be used to combat lung cancer. The treatment options for lung cancer are surgery, radiation therapy and chemotherapy. These may be used either alone or in combination depending on the type and stage of the tumor.
Optimally, non-small cell lung cancer is treated first with surgery if the disease is resectable and the patient a good candidate for surgery. If a lobe (section) of the lung is removed, the surgery is called a lobectomy. If the entire lung is removed, the surgery is called a pneumonectomy. While surgery may be the first step in treating your lung cancer, it may be considered after chemotherapy and radiation therapy. Sometimes radiation and chemotherapy will be delivered after the completion of your surgery, depending on the findings at surgery. If the tumor is not resectable or the person not a good medical candidate for surgery then a combination of radiation and chemotherapy is the treatment of choice.
Typically limited small cell lung cancer is treated with a combination of chemotherapy and radiation to the tumor. Chemotherapy refers to the use of drugs to kill cancer cells. Extensive stage small cell cancer is usually treated upfront with chemotherapy. Radiation is typically used in this stage of disease to relieve symptoms caused by the tumor in the chest or elsewhere in the body.
Radiation Therapy
Radiation therapy uses high energy rays (such as x-rays) to kill or shrink cancer cells. Radiation therapy works by damaging the ability of the cancer cells to multiply and divide. When the cells die, the body naturally eliminates them. Healthy cells are also effected by radiation. That is why there can be side effects during the course of treatment. However, normal cells have a greater capacity to repair themselves than cancer cells can. Therefore, the majority of side effect are temporary.
The high energy rays used to kill the cancer cells are usually delivered by a machine outside the body called a linear accelerator. This is called external beam irradiation. Radioactive materials can also be placed directly in the tumor called internal or implant radiation, also called brachytherapy. External radiation is the type most often used to treat lung cancer.
External beam irradiation is used as the main treatment of lung cancer for those who may not be healthy enough to have surgery or whose cancer has spread too far to be removed by surgery. Often, chemotherapy is given at the same time as the radiation. For other patients, radiation may be used after surgery to kill small areas of cancer that cannot be seen and removed during surgery. Radiation can also be used to relieve symptoms such as pain, bleeding, or blockage of air passages by the tumor. It is also a treatment of lung cancer that has spread to other organs such as the bone or brain.
External beam radiation therapy is usually given in daily doses, five days per week. The radiation may be delivered over a period of two to seven weeks depending on type and stage of the cancer.
Cancer doctors, called Radiation Oncologists, specialize in treating cancer with radiation therapy. They will decide how to deliver the radiation therapy to best target the tumor but avoid as much of the normal surrounding organs as possible. Your tumor may be treated with 3 Dimensional Conformal Radiation Therapy which combines multiple radiation treatment fields to deliver precise doses of radiation to the lung tumor. Tailoring each of the radiation beams to accurately target the tumor protects nearby healthy tissue. IMRT may also be used to treat your tumor. This is even a more sophisticated form of 3D treatment planning that modifies the radiation by varying the intensity of each radiation beam. This technique allows the precise adjustment of radiation doses to the tissue within the target area, possibly allowing a higher radiation dose to the tumor, and keeping more radiation away from nearby normal tissues. Tomotherapy® may also be used to treat your tumor. This is a new and revolutionary way of delivering radiation with a high-output linear accelerator mounted on a CT scan gantry which rotates about the patient in a helical pattern. The radiation beam consists of tiny “beamlets”, each of which strike the patient from a full 360 degrees. Each beamlet can be independently switched on or off at any time depending on whether it is pointed at tumor or normal tissue. Tomotherapy can improve the accuracy and precision of treatment.
For small lung tumors in patients with limited lung function and who are not good candidates for surgery, Stereotactic Body Radiation Therapy (SBRT) offers an exciting treatment alternative. Radiation treatment planning for SBRT is a very complex and exacting process, using specialized “4-dimensional” CT scans that take into account the exact motion of the tumor with breathing. Large, focused radiation doses to very small regions of the lung can be achieved, and tumor control and cure rates are very competitive with surgery. Treatments are non-invasive, and are usually completed within one week. ROA offers this treatment on our Trilogy and Tomotherapy machines, which are both capable of delivering this highly sophisticated therapy. Please see the Stereotactic Body Radiotherapy/SBRT section for more details.
Effective, safe and compassionate patient care is our top priority
Possible Side Effects
Side effects of radiation are limited to the area of the body that is treated. Side effects from radiation to the chest may include a mild skin reaction, cough, difficulty swallowing from irritation of the esophagus, and fatigue. These side effects are usually temporary. Most patients are able to continue their normal routine throughout the radiation.
Effective, safe and compassionate patient care is our top priority
Latest News
Dr. Lonika Majithia publishes on The Clinical Utility of DCISionRT on Radiation Therapy Decision Making in Patients with Ductal Carcinoma In Situ Following Breast-Conserving Surgery in Annals of Surgical Oncology
Abstract Background The role of radiation therapy (RT) following breast-conserving surgery (BCS) in ductal carcinoma in situ (DCIS) remains controversial. Trials have not identified a low-risk cohort, based on clinicopathologic features, who do not benefit from RT. A biosignature (DCISionRT®) that evaluates recurrence risk has been developed and validated. We evaluated the impact of DCISionRT […]
Dr. Avani Rao publishes on plan quality effects of proton therapy for central nervous system and skull base tumors in Radiotherapy and Oncology
Abstract Purpose With reports of CNS toxicity in patients treated with proton therapy at doses lower than would be expected based on photon data, it has been proposed that heavy monitor unit (MU) weighting of pencil beam scanning (PBS) proton therapy spots may potentially increase the risk of toxicity. We evaluated the impact of maximum […]
Dr. Daniel Kim publishes on the implications of practice consolidation among radiation oncologists
Abstract Purpose Health care practices across the United States have been consolidating in response to various market forces. The degree of practice consolidation varies widely across specialties but has not been well studied within radiation oncology. This study used Medicare data to characterize the extent of practice consolidation among radiation oncologists and to investigate associated […]
Cancer Types
Radiation Oncology Associates is the leader in comprehensive and cutting-edge radiation oncology therapy services in convenient and accessible locations across Northern Virginia.